The following interview was posted on Lyme.no, the website of the Norwegian Lyme Borreliosis Association, in 2010.
Dr. Bózsik is the inventor of DualDur and the leader of the Diagnostic & Therapeutic Workgroup of the Lyme Borreliosis Foundation, Hungary.
25 YEARS EXPERIENCE WITH LYME BORRELIOSIS
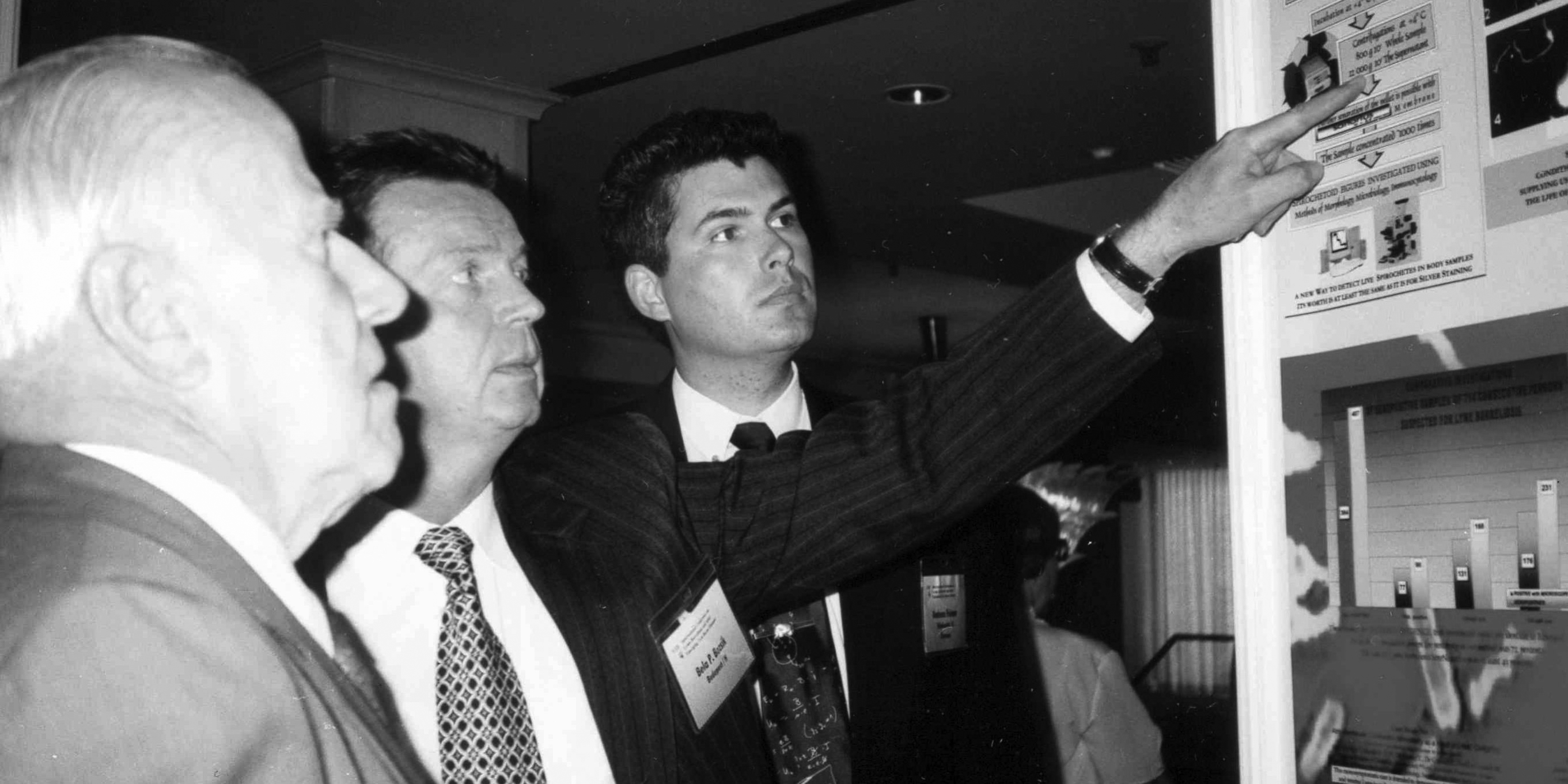
Dr. Bela P. Bozsik is a Hungarian physician with a unique experience in diagnostics and treatment of Lyme borreliosis. After the discovery of the Borrelia spirochete early in the eighties, Dr. Bozsik was soon engaged in work in the field. With his background from laboratory medicine, he had good insight in the development of test methods, and he soon understood that both diagnostics and treatment would face greater challenges than what was initially believed. During a recent stay in Budapest, we had the opportunity to meet Dr. Bozsik.
The bacterium Borrelia burgdorferi was identified in the USA in 1982, and was connected to an epidemic of arthritis among children in the small town Lyme a few years earlier. It was known that the bacterium was transmitted by ticks. In Europe there were observations that connected tick bites to the occurrence of the characteristic dermatological conditions EM and ACA, but the fact that this newly discovered spirochete was the causative agent of illness was new, also in Europe. Several scientists took interest in this new spirochete, and Dr. Bozsik was one of the first to engage in the field. He was the first to suggest the term Lyme Borreliosis, this was accepted and immediately taken into use.
What was your background, why did you go into the work with Lyme borreliosis?
The most interesting and promising aspect of this new discovery was that there is a disease that can damage the whole body, developing into a systemic disease, and the causative agent could be killed with common antibiotics. This gave an incomprehensible possibility to cure people suffering from obscure symptoms without known causes, so I decided to do research in this field. Before this I had been working with the complement system and serology in Syphilis diagnostics. The Syphilis bacterium is also a spirochete, and has many similarities to Borrelia. At this time I was head of the serology laboratory at Johan Bela National Institute of Hygiene. An infectious diseases specialist at the institute asked me to do something on the new spirochete, and we started to adapt methods for serological investigations.
We know that a bitter conflict has developed between wings, where physicians at either side have very different opinions on Lyme borreliosis. This has been very expressed in the USA. Unfortunately we have also found this conflict to be present in Europe.
How was the situation initially, when did this conflict start?
During the first years there were open- hearted and good conditions for work, and there was a friendly attitude at the international congresses. The scientists wished to share experiences and develop new knowledge. In short words; we fought with Lyme borreliosis and not with our Colleagues. In 1990, at the international conference in Stockholm, the conflict came to the surface. It was during a round-table discussion that developed to a fierce debate. It almost ended in a physical fight! At the time professor Klaus Weber from Munich, the president of the round-table discussion, closed the debate by saying “We are here to help patients suffering by Lyme borreliosis, not to fight each other”. The disagreement arose from the different opinions among the experts regarding what was the most efficient antibiotic for treatment of Lyme borreliosis.
The question regarding treatment is still a matter of debate, as we all know. Health authorities in almost every country suggest treatment according to guidelines from IDSA in the USA. This happens even though it is clear that the situation is very differing in Europe and USA. In Europe we have at least three substrains, perhaps five or more, of Borrelia that cause human illness. In the USA there is one strain that is dominating. Standard treatment for borreliosis in most countries is 2-4 weeks of monotherapy with ceftriaxone, doxycyklin, or eventually Penicillin V in early stages.
Dr. Bozsik, You have been a pioneer in the development of combined antibiotic therapy for Lyme borreliosis, can you say something about the background for this work?
It was obvious that monotherapy in many cases did not give a satisfactory result, and I started to think that the combination of different antibiotics could give a synergistic effect. With the help of colleagues in different Institutes I did some studies In vitro, with different strains of Borrelia in culture. We tested fluoroquinolone in combination with different other antibiotics like doxycyclin, clarithromycin etc. In all cases we saw a marked synergy, even though Dr. Wilske had presented In vitro-results at the Stockholm conference showing that ciprofloxacin was ineffective alone against Borrelia. We also saw that some patients had good effect of their treatment while others did not improve much. Professor Neubert presented results from In-vitro tests, showing that different Borrelia strains had different susceptibility to different types of antibiotics. Some time later, at the conference in Vienna in 2005, it was discussed with Brorson if tinidazole could be an efficient drug to include in the treatment regime, to target the Gemma (spheroplast, “cyst”-like stage).
The principle for the development of my treatment schedule has been to use ciprofloxacin in combination with another antibiotic to utilize the synergistic effect that was demonstrated in the laboratory studies, and in addition to include tinidazole for the Gemma. In our practice we saw that the patients had cyclic variation in their symptoms in periods of 3-4 weeks. The treatment period should last for 2-3 times the duration of the individual cycle for the patient; that is approximately 8 weeks. We experienced that clinical improvement could continue for a long time after ending the treatment, 2-4 moths even 6 monthes after. However, if the symptoms continue or flare up, the patient may need repeated treatment with a different antibiotic. It is important to know what strain of Borrelia the patient is infected with, in order to choose the best antibiotic for the treatment schedule
It was of course important to investigate the effect of the combined antibiotic treatment in a clinical practice, and not only in the laboratory. Initially I had contact with a Hungarian group of physicians who wanted to try this treatment schedule for some of their patients. Gradually we collected comprehensive data from a group of 250 patients suffering from chronic Lyme borreliosis here in Hungary. We followed these patients for 5 years, on average, and half of them were cured after one round of treatment, while others needed one or more repeated treatments. Nearly all of them were cured, not seeing the definitive pathoanatomic lesions. I have also realized that it is very important to strengthen the immune defense at the same time as giving the patient antibiotic treatment.
What the patients experience today is that it can be very difficult to get a correct diagnosis, to prove there is an ongoing Borrelia infection. The problem seems most severe for the long term ill patients. The experts accept that the immune response can be low in the early stage of the illness, but they claim that serologic testing is all reliable in the late stages of illness. In theory they can admit that seronegative borreliosis may exist, but they say it is extremely rare. In their everyday practice a negative test is used to rule out illness.
How do you think about these questions regarding interpretation and use of serologic tests, and eventual other test methods?
The experts have forgotten what it means in everyday practice that serology is an indirect diagnostic method. Seronegativity means that the method (!) cannot demonstrate the presence of antibodies, -for some or other reason. It does not mean that Lyme borreliosis is not there. One should know that there is a period in the early stage of illness where production of antibodies is low, but there is also such a period of low antibody production in the late stage. That is why it is very useful to have additional methods to demonstrate active infection. I have been working a lot with classical dark-field microscopy, and I realized there was a need for methods to distinguish between the spirochete and artefacts in the preparations. I have developed a reagent (DualDur) that is added to the blood sample. This reagent makes the other objects rigid and motionless and there are no artificial products, while the Borrelia are preserved and still moving normally.
Dr Bozsik is now retired, but he is still working full time as a volunteer in Lyme Borreliosis Foundation Hungary, an organization that he founded in 1991. He has close contact with patients, physicians and scientists in several countries, and spends his time helping others. His heart is with the patients, and on every Sunday he burns a candle for the Lyme patients and their physicians.
Written by Gerd Berge, Norwegian Lyme Borreliosis Association